Care Management
Making Healthcare Accessible
What is Care Management
- Care Management is a service to ensure effective coordination and management of care
- by ensuring all those involved in an individual’s care are working together to support a person’s recovery and overall health.
- It ensures members get the services they need to connect and get regular guidance from the assigned Care Manager on navigating the medical system in the United States.
- Care Management helps minimize preventable emergency department visits, establishing care with general practitioners and making sure members are developing a better relationship and understanding of the medical system overall

Care management roles
Building close relationships with patients and their medical care provider(s) by visiting patients in their homes.
Making medical appointments for patients and coordinating transportation to appointments and medication.
Discussing care plan to find areas for improvement by researching the legality of patient care plans and educating the client
Care Management at RISE
- Positive attitude
- Communication skills
- Negotiation skills
- Ability to provide emotional support
- Ability to delegate tasks
- Teamwork and collaboration
- Clinical skills
- Ability to network with medical professionals
What is our Program
Our program helps refugee and immigrant communities by assessing their healthcare needs and creating a personalized care plan. We work to coordinate the behavioral and physical healthcare needs of each patient by ensuring they are connected to the right healthcare providers. Our Care Managers work to connect members to services and providers such as physical therapists, specialty care practitioners, pharmacists, counselors (mental and health substance abuse), physicians, as well as social and legal aid, etc. Our Care Managers become advocates for the care recipients by conducting ongoing assessments and care plans to monitor and implement changes according to the individual needs of each client. Our care managers also assist with general care coordination by helping clients schedule medical appointments and partnering with the member’s doctor and a team of healthcare providers to help bridge gaps in healthcare connectivity.
RISE Care Management Benefits
- A dedicated care manager
- A comprehensive care plan
- Medication and care-management support
- A hospital-to-home program
- Patient education materials
- Expanded communication between patients and healthcare professionals
- Care coordination with community and home-based service providers
- Improved clinical outcomes
- Reduced use of high-cost acute care services
- More primary and/or preventive care visits
- Fewer duplicative tests and procedures
- Higher patient satisfaction
What makes RISE Care Management Unique?
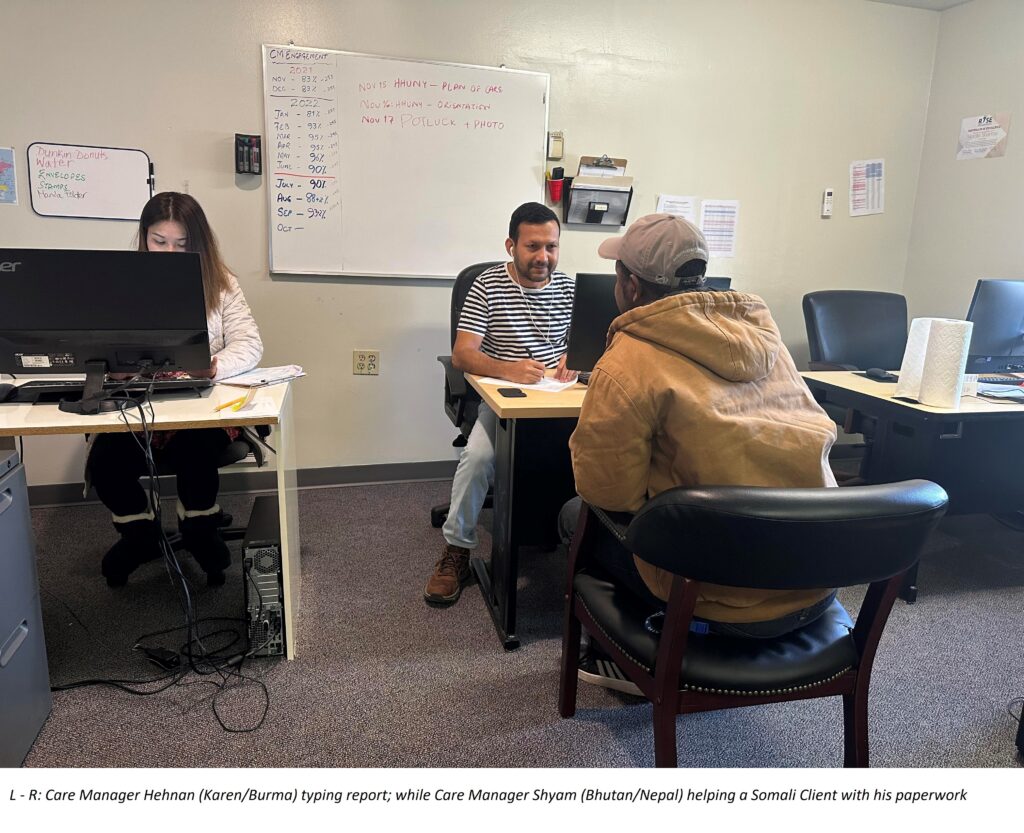
RISE Care Management aims to try and connect disadvantaged immigrant and refugee communities with as many services as possible by partnering them with a Care Manager that can speak their language. The Care Managers that RISE employs are respected community members that can communicate and navigate the complex cultural/social and language spheres of our clients. Currently, our Care Managers speak a combined total of 20+ unique languages and dialects, not including English. Our overall goal is to make healthcare more accessible to disadvantaged communities through the efforts of our Care Managers to build a partnership of trust with our clients. RISE Care Managers works with the diverse web of programs that RISE offers to connect clients to Bridging Case Managers, Employment Assistance, Education Coordinators, and IDA Program assistance. Ideally, our clients as well as their family members will be able to receive support in many different areas of their lives apart from just healthcare connectivity.
Who do we partner with?
- St. Joe’s Care Coordination Network (SJCCN)
- Health Home of Upstate New York (HHUNY)
- Molina
- Fidelis
- Excellus
- Humana
- United Healthcare.
Eligibility Requirement
- To be eligible for health home services, an individual must be enrolled in Medicaid or Medicare.
- An individual must have two or more chronic conditions or one single qualifying chronic condition
- Two or more chronic conditions may include asthma, diabetes, mental health conditions, heart disease, substance abuse disorders, obesity, etc.
- Single qualifying chronic conditions, according to New York State are HIV, and Serious Mental Illness (SMI)
- Individuals must also have significant social risk factors, including inadequate housing, lack of access to transportation or food, non-adherence to treatments and medications, high ER usage, lack of healthcare connectivity, a recent release from incarceration, and lack of social/family support.
